Disability Inclusive Curriculum
Disability Equality in Education
 The Disability Equality in Education (DEE) organization is a cross-disability led non-profit organization that initiated efforts to implement a Disability Inclusive Curriculum in schools. Pennsylvania is the first state to introduce the curriculum, which DEE hopes will eventually take place in all schools nationwide.
The Disability Equality in Education (DEE) organization is a cross-disability led non-profit organization that initiated efforts to implement a Disability Inclusive Curriculum in schools. Pennsylvania is the first state to introduce the curriculum, which DEE hopes will eventually take place in all schools nationwide.
The ‘Disability Inclusive Curriculum’ will help K-12 students understand that disabilities are natural by embedding representation and lessons about people with disabilities throughout the general education curriculum, activites and environments. It includes teaching students about the political economic, and social contributions by people with disabilities.
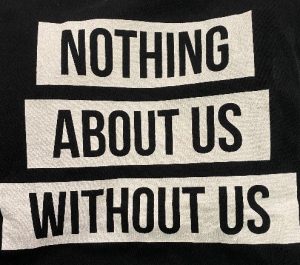
DEE brings a unique perspective and expertise on disability in to the educational setting because of contributions by their network of disabled people and advocates from around the world. “Nothing About Us Without Us” is the heart of who they are and what they do.
A comprehensive ‘Disability Inclusive Curriculum Lesson Plan Library‘ was created by DEE and is available on their website as a resource for teachers to explore disability in the classroom. The focus is to normalize the idea of disability with all students.
In Pennsylvania
To learn more about the pilot program in Pennsylvania visit Pennsylvania’s Disability Inclusive Curriculum Pilot Program. Schools can apply for up to $30,000 in grant funding available through the Pa Department of Education to implement disability inclusive curriculum. Funding will be granted to successful applicants for a three-year period from the date of the award through June 30, 2026. A maximum of $10,000 per year is available to each school entity or nonpublic school entity. Grant applications are due by May 15th, 2023. There is also a webinar overview of the grants and Q & A’s at https://www.pattan.net/Supports/Inclusive-Practices
Support DEE and the Disability Inclusive Curriculum


-

- Send checks: “DEE” 3607 Windsor Drive, Bensalem, PA 19020
- Help DEE get connected with grants and donors for funding
- Network with DEE and talk to leaders and advocates in your state
- Contact DEE info@disabilityequalityeducation.org
- Visit the DEE website
- Join the DEE Education Forum on Facebook
- Share this initiative with others to help and support DEE and the implemention of Disability Inclusive Curriculum.
Your support can make teaching a ‘Disability Inclusive Curriculum’ to all students in all schools across the nation possible!
Additional links: